Sharon,
It sounds to me that your brain is playing tricks on you. Your nerve endings are gone, yet you still feel pain. It sounds like a neuroplasticity problem. There are researchers/doctors who have devised methods of "retricking" the brain in cases of chronic pain with no organic cause, such as phantom limb pain. For instance, using a mirror to show the patient his good hand, yet making the patient believe that it is his phantom hand. Once the patient can see himself moving the phantom hand, unclenching it, and shaking it, the phantom pain disappears. (This takes place over several sessions.)
I am in the midst of reading a fascinating book about the subject of neuroplasticity, written by a Toronto psychiatrist named Norman Doidge, The Brain that Changes Itself: Stories of Personal Triumph from the Frontiers of Brain Science. It comes in softcover, and I bought it on Amazon. The story of the phantom hand is in Chapter 7 titled "Pain - The Dark Side of Plasticity". There is also a YouTube documentary featuring Dr. Doidge which was recently broadcast on the Canadian TV science show, the Nature of Things, with David Suzuki. It's in three segments and is about 45 minutes long.
Maybe you could get in touch with some of the doctors mentioned in the book/documentary and see if they will take you on as a patient. Most of them are in the United States.
Thinking of you.
Dr Dellon
Re: Dr Dellon
Athlete until pain started in 2001. Diagnosed with PN in Nov. 2010. Probable cause: 3 difficult labors, 5 pelvic surgeries for endometriosis, and undiagnosed hip injuries. 60% better after 3 rounds of shockwave therapy in Cornwall, Ontario (Dec - Feb/12). 99% better after bilateral hip scopes for FAI and labral tears (April and July/12). Pelvic pain life coach Lorraine Faendrich helped me overcome the mind/body connection to chronic pain: http://www.radiantlifedesign.com
-
LottaNerve
- Posts: 164
- Joined: Fri Sep 24, 2010 8:56 am
- Location: Central California
- Contact:
Re: Dr Dellon
Lernica,
Yeah! I've seen the video from TED Talks showing the mirror therapy for phantom limb pain by the doctor who invented it. Fascinating, wonderful stuff.
I have a friend who had her bladder removed years ago due to end-stage Interstitial Cystitis. She still "feels" her inflamed bladder.
Yeah! I've seen the video from TED Talks showing the mirror therapy for phantom limb pain by the doctor who invented it. Fascinating, wonderful stuff.
I have a friend who had her bladder removed years ago due to end-stage Interstitial Cystitis. She still "feels" her inflamed bladder.
http://www.icandpne.wordpress.com
1995 First symptoms of PNE and IC
8/2010 Dr. Hibner, left TG- failed surgery.
3/2011 & 10/2011 - Dr. Dellon, left dorsal/perineal neurolysis -also failed.
1/2012 3-day ketamine infusions. Pain-free for several days! Bladder flared from IC.
11/2012 Intrathecal pain pump (bupivacaine, clonidine, morphine) Dr. Joshua Prager, UCLA.
2/13 My pain is reduced!
5/15 Living life again!
1995 First symptoms of PNE and IC
8/2010 Dr. Hibner, left TG- failed surgery.
3/2011 & 10/2011 - Dr. Dellon, left dorsal/perineal neurolysis -also failed.
1/2012 3-day ketamine infusions. Pain-free for several days! Bladder flared from IC.
11/2012 Intrathecal pain pump (bupivacaine, clonidine, morphine) Dr. Joshua Prager, UCLA.
2/13 My pain is reduced!
5/15 Living life again!
Re: Dr Dellon
Sharon,
At p. 192 of the same book, Dr. Doidge refers to the TENS unit and to acupuncture as possible solutions to end pain "even after its original stimulus has stopped". He writes:
"The gate theory led to new treatments for blocking pain. [Dr.] Wall coinvented "transcutaneous electrical nerve stimulation," or TENS, which uses electric current to stimulate neurons that inhibit pain, helping in effect close the gate. The gate theory also made Western scientists less skeptical of acupuncture, which reduces pain by stimulating points of the body often far from the site where the pain is felt. It seemed possible that acupuncture turns on neurones that inhibit pain, closing gates and blocking pain perception."
Maybe post-surgery is a good time for someone who still experiences pain to try TENS or acupuncture. Have you tried these recently?
At p. 192 of the same book, Dr. Doidge refers to the TENS unit and to acupuncture as possible solutions to end pain "even after its original stimulus has stopped". He writes:
"The gate theory led to new treatments for blocking pain. [Dr.] Wall coinvented "transcutaneous electrical nerve stimulation," or TENS, which uses electric current to stimulate neurons that inhibit pain, helping in effect close the gate. The gate theory also made Western scientists less skeptical of acupuncture, which reduces pain by stimulating points of the body often far from the site where the pain is felt. It seemed possible that acupuncture turns on neurones that inhibit pain, closing gates and blocking pain perception."
Maybe post-surgery is a good time for someone who still experiences pain to try TENS or acupuncture. Have you tried these recently?
Athlete until pain started in 2001. Diagnosed with PN in Nov. 2010. Probable cause: 3 difficult labors, 5 pelvic surgeries for endometriosis, and undiagnosed hip injuries. 60% better after 3 rounds of shockwave therapy in Cornwall, Ontario (Dec - Feb/12). 99% better after bilateral hip scopes for FAI and labral tears (April and July/12). Pelvic pain life coach Lorraine Faendrich helped me overcome the mind/body connection to chronic pain: http://www.radiantlifedesign.com
Re: Dr Dellon
Karyn, it was my understanding that Dr. Conway is one of the few surgeons who does follow-up so that's too bad he is not in your case. Was he unaware of his initial surgery results when he traveled to two other docs to learn a different approach?Karyn wrote: With all due respect, I'm not quite sure I understand how coming back to the forum and complaining to eachother is helpful. I think it would be more important to report our situations to the doctors to get their feedback and medical help. Yes, it's true that follow up takes time and $$$$$$ - something none of us have enough of. However, that coming from a surgeon .... MY surgeon for instance, is lame. It's half-ass care. Not enough time or money isn't a good enough excuse to not return phone calls or keep track of the surgeries you performed. To find out what else could be going on, instead of just deeming the surgery a failure. No room for a learning experience there!
I agree with you that typically with PNE there is more than just one issue going on - at least that's what most people seem to report.
You are right, we need to give feedback to the docs also and I think we can do that via e-mail or letters as I have done personally.
I learned about the association between pelvic instability and PNE from reading the forums and I took that information to two of the PNE surgeons who did not seem very aware of it. At least one subsequently altered his surgical approach although I can't say whether it was because of what I had told him. I could be wrong but I think some of the stuff we share here does get back to the docs and in the end helps to improve the quality of care that we receive. Of course more research would be great! We need to all work together to try to improve the quality of research.
PNE since 2002. Started from weightlifting. PNE surgery from Dr. Bautrant, Oct 2004. Pain now is usually a 0 and I can sit for hours on certain chairs. No longer take medication for PNE. Can work full time and do "The Firm" exercise program. 99% cured from PGAD. PNE surgery was right for me but it might not be for you. Do your research.
-
LottaNerve
- Posts: 164
- Joined: Fri Sep 24, 2010 8:56 am
- Location: Central California
- Contact:
Re: Dr Dellon
Lernica,Lernica wrote: Maybe post-surgery is a good time for someone who still experiences pain to try TENS or acupuncture. Have you tried these recently?
Yes, I have two TENS units, different brands, that i have used during flares for the past 10 years or so. They don't do much for me. Likewise, with acupuncture, I have had no positive response, and I have been to an acupuncturist who specializes in IC. She is in the LA area and I tried her program for nearly a year with no results. I really gave non-invasive therapies my best shot, from acupuncture to special diets (for my IC) to chiropractic. I even went to the 6-day Wise-Anderson clinic at great expense to learn relaxation techniques and have daily physical therapy, which was not helpful AT ALL - It made me feel like if I could only meditate and relax good enough, I could recover. After a year of following the protocol and listening to the relaxation tapes, I was no better, in fact, I was continuing to get worse, plus I was severely depressed because I felt like I wasn't "spiritual enough" to ever recover. That kind of thinking was toxic for me. It wasn't my fault I had IC and pudendal nerve entrapment; I hadn't caused it, and I had no control over it. So I moved on with nerve blocks, botox, and continued physical therapy, until I finally decided to try surgery.
I feel really good about the next direction I am going in -- Dr. Dellon is referring me to a specialist who I chose myself - Dr. Joshua Prager at UCLA. He has been featured in the ICA Update, a publication by the Interstitial Cystitis Association, and has helped many pelvic pain patients who have IC, like me. He leads a pain management team with many tools available to treat different kinds of pain and I am excited to see what he would advise in my situation. It is also time to address my pain more aggressively - it has become the monster in my life. I am feeling the possibility of getting some quality of life back!
http://www.icandpne.wordpress.com
1995 First symptoms of PNE and IC
8/2010 Dr. Hibner, left TG- failed surgery.
3/2011 & 10/2011 - Dr. Dellon, left dorsal/perineal neurolysis -also failed.
1/2012 3-day ketamine infusions. Pain-free for several days! Bladder flared from IC.
11/2012 Intrathecal pain pump (bupivacaine, clonidine, morphine) Dr. Joshua Prager, UCLA.
2/13 My pain is reduced!
5/15 Living life again!
1995 First symptoms of PNE and IC
8/2010 Dr. Hibner, left TG- failed surgery.
3/2011 & 10/2011 - Dr. Dellon, left dorsal/perineal neurolysis -also failed.
1/2012 3-day ketamine infusions. Pain-free for several days! Bladder flared from IC.
11/2012 Intrathecal pain pump (bupivacaine, clonidine, morphine) Dr. Joshua Prager, UCLA.
2/13 My pain is reduced!
5/15 Living life again!
-
LottaNerve
- Posts: 164
- Joined: Fri Sep 24, 2010 8:56 am
- Location: Central California
- Contact:
Re: Dr Dellon
I’m with you on that, Karyn. It sure isn’t helpful to us when we are put in a box marked “failed surgeries” and left to fend for ourselves. I recently found out that Dr. Dellon is going to start doing follow-up studies, thankfully. Also, when I had my surgery with Dr. Hibner, I was told that he is using interns to track surgical results. However, I was never contacted as far as my progress after surgery, so I don’t know if that is actually happening. I have a letter ready to send to him next week, so he will know I consider myself among the 1 percent of patients who get worse after his surgery.Karyn wrote: However, that coming from a surgeon .... MY surgeon for instance, is lame. It's half-ass care. Not enough time or money isn't a good enough excuse to not return phone calls or keep track of the surgeries you performed. To find out what else could be going on, instead of just deeming the surgery a failure.
I think he did the only thing he could do in the situation, other than send me somewhere for guided nerve blocks (which we discussed at one point).Karyn wrote: Sharon, my heart goes out to you. I'm deeply saddened Dr. Dellon cut you loose because of a failed nerve block. Could he have been wrong about his initial diagnosis?
Here’s what happened: After he did the first two injections in my backside, he left the room for about 10 minutes while they were supposed to take effect. During that time I got my ice packs out and when he walked back in the room I was laying on the table and holding ice between my legs. He looked at me, baffled. “Why are you using ice there?” he asked me. “Because it hurts!” I said, and by this time the tears were starting because my pain was really shooting up and I rarely go without my ice for very long.
I had emailed him about the pain returning, but I guess he didn’t really “get it” until he saw me suffering with his own eyes. So he changed gears and did the last injection into my left vulva where I was icing my pain. I didn’t get any relief from that 3rd injection either. I remember the look on his face and the way his shoulders kind of dropped when he finally understood. Here I was, in tremendous pain in an area where he had already operated on me twice, and removed or decompressed every nerve. That’s when he said, “I think you may be having central nervous system pain, and should consider sacral stimulation.”
Yes, my obturator, piriformis and all my pelvic floor muscles were evaluated when I had physical therapy with botox and trigger point injections for about a year and a half. I also had an MRI of my pelvis and my back, a laparoscopy to check my “female parts,” a cystoscopy to look inside my bladder (which we already knew had IC), and a colonoscopy to check my colon (perfectly healthy-looking). I am the healthiest sick person my doctors have ever seen. Except that the word “spastic” kept coming up. Bladder spasms. Bowel spasms. Everywhere spasms. So it is making sense to me that the problem is my CNS and brain coordination -- my nerves aren’t working right.Karyn wrote: None of my blocks OR infusions relieved my pain. Has your obturator been investigated?
http://www.icandpne.wordpress.com
1995 First symptoms of PNE and IC
8/2010 Dr. Hibner, left TG- failed surgery.
3/2011 & 10/2011 - Dr. Dellon, left dorsal/perineal neurolysis -also failed.
1/2012 3-day ketamine infusions. Pain-free for several days! Bladder flared from IC.
11/2012 Intrathecal pain pump (bupivacaine, clonidine, morphine) Dr. Joshua Prager, UCLA.
2/13 My pain is reduced!
5/15 Living life again!
1995 First symptoms of PNE and IC
8/2010 Dr. Hibner, left TG- failed surgery.
3/2011 & 10/2011 - Dr. Dellon, left dorsal/perineal neurolysis -also failed.
1/2012 3-day ketamine infusions. Pain-free for several days! Bladder flared from IC.
11/2012 Intrathecal pain pump (bupivacaine, clonidine, morphine) Dr. Joshua Prager, UCLA.
2/13 My pain is reduced!
5/15 Living life again!
-
LottaNerve
- Posts: 164
- Joined: Fri Sep 24, 2010 8:56 am
- Location: Central California
- Contact:
Re: Dr Dellon
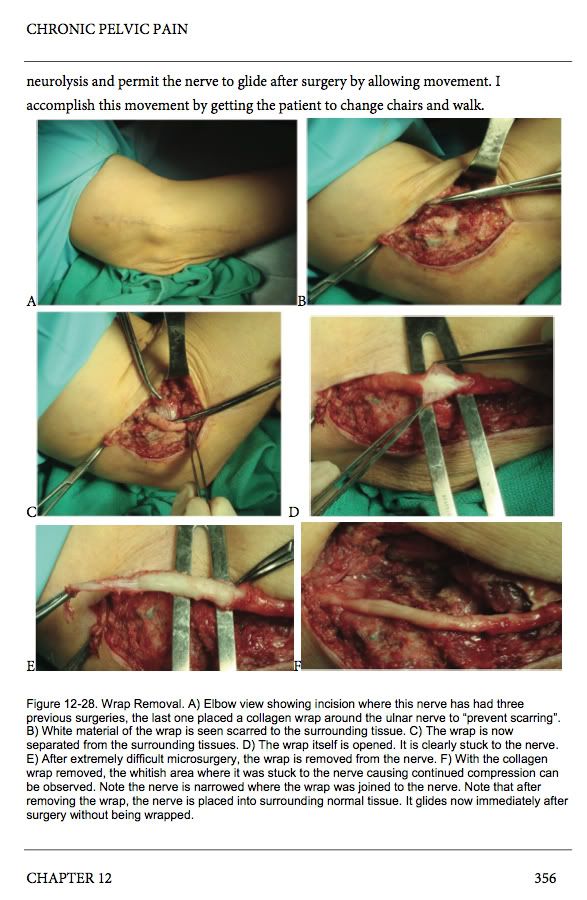
Karyn, I also wanted to respond to your note about neurawrap... I thought the same thing, that it dissolved a short time naturally after surgery. The marketing material for it is very compelling and I liked the idea of my nerve being "protected" and safe from further adhesions.Karyn wrote: It doesn't appear Dr. Dellon is aware that neurowrap completely dissolves within 2 weeks.
However, when I read Dr. Dellon's book, there is a section where he discussed neurawrap, called "Why I am not a wrapper." He has had to remove neurawrap where it has become almost “glued” to patients’ nerves --- it has not dissolved and can even cause further compression of the nerve.
What he writes about it is cautionary enough, but when I saw the photos I really wished I didn't have neurawrap inside of me.
It is in Chapter 12 on pages 354-357. Here is page 356.
I brought this up on another thread when I first read about it, but so far I'm the only one concerned about it that I know of....
http://www.icandpne.wordpress.com
1995 First symptoms of PNE and IC
8/2010 Dr. Hibner, left TG- failed surgery.
3/2011 & 10/2011 - Dr. Dellon, left dorsal/perineal neurolysis -also failed.
1/2012 3-day ketamine infusions. Pain-free for several days! Bladder flared from IC.
11/2012 Intrathecal pain pump (bupivacaine, clonidine, morphine) Dr. Joshua Prager, UCLA.
2/13 My pain is reduced!
5/15 Living life again!
1995 First symptoms of PNE and IC
8/2010 Dr. Hibner, left TG- failed surgery.
3/2011 & 10/2011 - Dr. Dellon, left dorsal/perineal neurolysis -also failed.
1/2012 3-day ketamine infusions. Pain-free for several days! Bladder flared from IC.
11/2012 Intrathecal pain pump (bupivacaine, clonidine, morphine) Dr. Joshua Prager, UCLA.
2/13 My pain is reduced!
5/15 Living life again!
Re: Dr Dellon
Wow, those are pretty powerful pictures, and so is your description of what happened to you. It sounds like it was a good thing Dr. Dellon did not go in and do anymore surgeries, knowing that it would probably not work for you. Did he have any experience or thoughts about ketamine?
PNE since 2002. Started from weightlifting. PNE surgery from Dr. Bautrant, Oct 2004. Pain now is usually a 0 and I can sit for hours on certain chairs. No longer take medication for PNE. Can work full time and do "The Firm" exercise program. 99% cured from PGAD. PNE surgery was right for me but it might not be for you. Do your research.
Re: Dr Dellon
Hi,
I do not come on this forum very often as my PN has gotten so better since I had Tarlov Cyst Surgery one year ago.
I still have some issues - mainly upregulation of CNS ie central sensitization, most likely from untreated PN pain for 1.5 yrs before I was dxed with Tarlov Cyst Disease.
Dr Dellon does not believe in central sensitization, and if a surgery isn't better in 4 months it was a failure.
His words.
My only remaining issues are inner thigh burning with exercise/ clothes and some vulvar pain that is moatly easily managed with lidocaine. All my inner pain, you guys know what I speak of!! and bowel bladder is gone.
Because I had bilateral hernia repair and my PT saw a lecture by Dr Dellon and he lives near enough to me, it was suggested I get his opinion on possibly removing the nerves going to my inner thighs thus allowing me a complete recovery.
I am not one to post bad things about any Dr as ,
I would hate to influence anyone who might be helped, so please take this with a grain of salt.
This was just my experience.
However, as Dr Dellon refuses to deal with insurance and my experience was so unprofessional, I feel it is my duty to share how my evel with him went.
Firstly, his wife ( as I found out later) does the ( or did mine) phone eval to clear me to see him.
She spoke as a professional and said most definately that I was a candidate to see him.
We talked for over an hour....to my delight ..( have to wonder about this one...and what it means)
he had an opening the next week.
She said that no he doesn't take insurance ..but that I could submit papers to my insurance and get reimbursed. When we arrived we discovered that he specifically opted out of numerous insurances ,
mine included and I would not be allowed or given a form to send back.....so we had to decide on the spot whether or not to give him $750. for his opinion.
We argued over this and ...then the ....( wife) said .... something different, and that insurance should make no difference.....because of what my husband did for a living..that Dr Dellon would take care of me ect ect.... please let him try!! ect ect
We asked how much surgery would be....$30,000 +-
...but she talked us into the exam room with the same
promise he could help ect....
the first thing out of his month was " What is your education level?" ( I have a masters' degree)
Then he spent most of the exam , teaching me anatomy !!! and explaining how bad my NS did his job.
after all that he said that he could scrub in to re-do my original surgery!
One that he has no experience whatsoever in....
the topper was he dragged us to the next room to see a surgery success....a young girl who he removed a nerve in her foot. so she would not have foot pain!!
He described how devasting her pain was??????
the exam was very small portion of the visit. 10-15 mins of 75-90mins.
I tried to explain that I felt better the first 3 months but when the pelvic girdle numbness receded,
that I had some remaining issues.
The vast majority is so much better or gone, but these issues were still quality of life issues..ie sex and walking/wearing pants comfortably.
the kicker was he had the nerve to say.....after I said I had success with lidocaine (vulvar)and a pudendal
blocks for short periods ... He smirked and said. " Oh you are one that likes feeling numb"
The entire visit felt very condescending, and I said to my husband as we drove the 2 hrs home that he has no intention of ever helping us, even if he could , because we don't have that kind of money......
his wife said the opposite yet again on our way out the door...but whatever.
Sure enough, he retracted most of what he said in a letter 10 days later, saying he rethought my situation and could not help. So I was out the $750- okay ( not) but i was prepared for that,
Please do see him if you think he can help, guys might do better than women.
My saving grace was I prayed on the way there for the universe to make it clear whether or to have surgery with him. The answer was more than clear!
Sorry for the negative- that is not like me.
Hope that I did not break any forum rules, if so apologize in advance and can remove the post if need be.
yoland
This post has been edited by the moderators to remove obscene language.
I do not come on this forum very often as my PN has gotten so better since I had Tarlov Cyst Surgery one year ago.
I still have some issues - mainly upregulation of CNS ie central sensitization, most likely from untreated PN pain for 1.5 yrs before I was dxed with Tarlov Cyst Disease.
Dr Dellon does not believe in central sensitization, and if a surgery isn't better in 4 months it was a failure.
His words.
My only remaining issues are inner thigh burning with exercise/ clothes and some vulvar pain that is moatly easily managed with lidocaine. All my inner pain, you guys know what I speak of!! and bowel bladder is gone.
Because I had bilateral hernia repair and my PT saw a lecture by Dr Dellon and he lives near enough to me, it was suggested I get his opinion on possibly removing the nerves going to my inner thighs thus allowing me a complete recovery.
I am not one to post bad things about any Dr as ,
I would hate to influence anyone who might be helped, so please take this with a grain of salt.
This was just my experience.
However, as Dr Dellon refuses to deal with insurance and my experience was so unprofessional, I feel it is my duty to share how my evel with him went.
Firstly, his wife ( as I found out later) does the ( or did mine) phone eval to clear me to see him.
She spoke as a professional and said most definately that I was a candidate to see him.
We talked for over an hour....to my delight ..( have to wonder about this one...and what it means)
he had an opening the next week.
She said that no he doesn't take insurance ..but that I could submit papers to my insurance and get reimbursed. When we arrived we discovered that he specifically opted out of numerous insurances ,
mine included and I would not be allowed or given a form to send back.....so we had to decide on the spot whether or not to give him $750. for his opinion.
We argued over this and ...then the ....( wife) said .... something different, and that insurance should make no difference.....because of what my husband did for a living..that Dr Dellon would take care of me ect ect.... please let him try!! ect ect
We asked how much surgery would be....$30,000 +-
...but she talked us into the exam room with the same
promise he could help ect....
the first thing out of his month was " What is your education level?" ( I have a masters' degree)
Then he spent most of the exam , teaching me anatomy !!! and explaining how bad my NS did his job.
after all that he said that he could scrub in to re-do my original surgery!
One that he has no experience whatsoever in....
the topper was he dragged us to the next room to see a surgery success....a young girl who he removed a nerve in her foot. so she would not have foot pain!!
He described how devasting her pain was??????
the exam was very small portion of the visit. 10-15 mins of 75-90mins.
I tried to explain that I felt better the first 3 months but when the pelvic girdle numbness receded,
that I had some remaining issues.
The vast majority is so much better or gone, but these issues were still quality of life issues..ie sex and walking/wearing pants comfortably.
the kicker was he had the nerve to say.....after I said I had success with lidocaine (vulvar)and a pudendal
blocks for short periods ... He smirked and said. " Oh you are one that likes feeling numb"
The entire visit felt very condescending, and I said to my husband as we drove the 2 hrs home that he has no intention of ever helping us, even if he could , because we don't have that kind of money......
his wife said the opposite yet again on our way out the door...but whatever.
Sure enough, he retracted most of what he said in a letter 10 days later, saying he rethought my situation and could not help. So I was out the $750- okay ( not) but i was prepared for that,
Please do see him if you think he can help, guys might do better than women.
My saving grace was I prayed on the way there for the universe to make it clear whether or to have surgery with him. The answer was more than clear!
Sorry for the negative- that is not like me.
Hope that I did not break any forum rules, if so apologize in advance and can remove the post if need be.
yoland
This post has been edited by the moderators to remove obscene language.
Re: Dr Dellon
Yoland, thanks for taking the time to share your experience with Dr. Dellon. Not a flattering portrait, that's for sure. It's really important that we get to hear all points of view so everyone can process it all as we try to figure out our next move.
Don
Don
Mild to moderate PN for 5 plus years, pain controlled by lyrica and opiates.
Nerve block (unguided) 9/10 Dr. Jerome Weiss - sciatica for 5 months but got numb in painful perineal/scrotal area - he diagnosed entrapment - but no more cortisone for me
Potter MRI 5/11 - rt STL entrapment of PN at Alcocks
Consult with Dr. Hibner Feb. 2012
Bilateral inguinal hernias diagnosed by dynamic ultrasound - surgery on 6/20/13
Feeling a little better, a few more months will tell
Nerve block (unguided) 9/10 Dr. Jerome Weiss - sciatica for 5 months but got numb in painful perineal/scrotal area - he diagnosed entrapment - but no more cortisone for me
Potter MRI 5/11 - rt STL entrapment of PN at Alcocks
Consult with Dr. Hibner Feb. 2012
Bilateral inguinal hernias diagnosed by dynamic ultrasound - surgery on 6/20/13
Feeling a little better, a few more months will tell