Frequently Asked Questions
The answers to these questions were written by veteran PNE sufferers but we are not doctors. For a fuller and more reliable description of pudendal neuralgia please see the literature and your doctor. As you read the FAQ’s on this page keep in mind that PN and PNE are not used interchangeably since PNE refers to a more specific problem than PN.
-
1. How do I know if I have pudendal neuralgia (PN)?
If you have pain in the pudendal nerve distribution area and doctors cannot find a reason for it then you might have pudendal neuralgia. The pudendal nerve innervates the penis and clitoris, bulbospongiosus and ischiocavernosus muscles, and areas around the scrotum, perineum, and anus. (
see anatomy section) The pain can be burning, stabbing, aching, or just a sense of numbness with loss of sensation. Sometimes the pain is mild and comes and goes for several months or years. Sometimes the pain hits suddenly and never goes away. Sometimes it just comes on slowly and gets worse over time. Sometimes you can associate the start of the pain with a traumatic event or pelvic surgery. Each case is different.
2. What is the difference between pudendal neuralgia (PN), pudendal neuropathy, and pudendal nerve entrapment (PNE)?
While the medical community is still in the process of defining some of these terms exactly, there is some agreement on what the terms mean. Neuralgia is typically thought of as pain along the course of a nerve due to inflammation. Neuropathy is associated with a pathology or functional disturbance in the nerve. These two terms are very closely related and sometimes used interchangeably. Often these terms are abbreviated as PN in the pudendal community.
Pudendal nerve entrapment (PNE) is a more specific term describing a neuropathy or neuralgia that is associated with the nerve being tethered by fascia, compressed by ligaments, enlarged muscles, and/or other structures. Sometimes the nerve is restricted so that it cannot glide easily resulting in a stretch or tension injury to the nerve. Generally if the nerve is impinged upon by tight, tense muscles it is not considered a true entrapment because surgical intervention is not required to relieve the impingement. If the impingement is due to tight muscles, physical therapy might help relieve the tension.
3. What is pudendal nerve entrapment (PNE)?
Pudendal nerve entrapment (PNE) is a condition causing pain for no apparent reason in the lower central pelvic areas. These are the anal region, perineum, scrotum and penis, vulva and clitoral areas. Pain is worse upon sitting and less when standing or sitting on a donut cushion or toilet seat. But there is no one particular pattern that dominates. Pain can be in just one area, several, or all. It can be unilateral or bilateral (on one side or both sides). In some cases standing will relieve the pain but lying down will not. However the pain can be present in any position.
Because pudendal neuralgia is nerve related, some of the pain that is felt might be different from regular muscular pain. Pudendal neuralgia sufferers usually describe their pain as stinging, burning, stabbing, aching, knife-like, irritation, cramping, spasm, tightness, crawling on the skin, twisting, pins and needles, numbness, and hyper- sensitivity. As Prof Roberts writes, “The character of the pain consists of sensations of burning, torsion or heaviness, and also of foreign bodies in the rectum or vagina. The pain is piercing and very comparable to a toothache.” The pain may feel shallow or deep. It often starts in one place and progresses.
Frequently there is also urinary, anal, or sexual dysfunctionality. There are many other pain areas associated with PNE, such as internal organs or pain radiating down the leg. However, if pain is not present in the “classic” areas, the condition is less likely to be PNE. It may be another nerve, such as the cutaneous, or it may not be nerve damage related at all.
As Professor Robert writes:
“The main daily activities requiring the seated position (work, meals, driving, theaters, etc) are no longer available to these patients, whose mental attitude is one of chronic pain sufferers so obsessed with their miserable state as to be rapidly regarded by their doctors as psychiatric cases.”
Prof. Robert and his team have published an
article outlining the criteria they believe points to PNE.
The pain is sometimes so intense that suicide is considered. But since a change of day to day habits can alleviate the pain some or a lot, people make those changes and usually learn to tolerate the pain that remains. Some cases have gone on for 20 years. Many seem to be in the 5 to 10 year range, apparently because that’s how long it takes on the average to stumble onto a doctor that can correctly diagnose PNE.
Strictly speaking, PNE is a subset of pudendal neuralgia or pudendal neuropathy (PN). Neuropathy is nerve disease or damage. PNE involves entrapment, while PN involves entrapment, disease, or damage of any kind. In your initial diagnostic stages it’s more useful to think PN. As tests become definite and point to entrapment, it is time to think PNE.
PN can be caused by an injury to the nerve or any disease of the nerve that causes inflammation or demyelination of the nerve. Some people have associated their PN symptoms with post-herpetic neuralgia, Lyme’s disease, multiple sclerosis, or other autoimmune illnesses. Other people can point to an injury or pelvic surgery as the start of their symptoms. Heavy exercise is considered one of the causes of PN. Activities that require repetitive hip flexion such as cycling and weightlifting can be the culprit. Jobs that require heavy lifting or many hours of sitting may be the cause.
“The pudendal nerve comes from the sacral plexus (S2-S4) and enters the gluteal region through the lower part of the greater sciatic foramen. It courses through the pelvis and around the ischial spine and between the sacrospinous and sacrotuberous ligaments. It splits up into the rectal, anal, perineal and clitoral/penis branches.The nerve turns forward and downwards through the lower sciatic foramen underneath the surface of the levator muscle into the Alcock’s canal where the nerve is flattened out between this double fascia (aponeurosis). The two most important narrow passages are around the ischial spine between the sacrospinous and the sacrotuberous ligaments (80%) and in the Alcock’s canal (20%). Cycling, riding and long drives can kick off the symptoms of pudendal neuralgia” (Referenced from a Mayo Clinic article)
PNE is caused by entrapment of the pudendal nerve at any of various places on the nerve. Nerve entrapment occurs when a nerve is constricted for some reason and responds by inflammation, scarring, or thickening. These can cause nerve diameter to increase and the nerve to misbehave.
The initial constriction is caused by pressure or trauma of some type or an unknown reason. If this occurs where a natural constriction is also present, such as where the nerve passes over a bone or through a tunnel, then once the nerve increases in size a vicious cycle can begin. As the nerve swells it encounters a natural constraint. This increases prolonged pressure on the nerve, which causes more swelling, which causes more pressure, and so on. This vicious cycle explains why the pain can go from a low to a high level so fast, and why once a case becomes chronic, very little sitting, no sitting at all, or the least bit of movement can elicit pain.
Entrapment is a bit of a catch-all term. Stretching or rubbing of the pudendal nerve can also cause PNE. In all cases the result is nerve irritation, which causes improper functioning of the nerve. An entrapped nerve misreports pain and causes organ dysfunctionality such as urinary, defecation, and sexual problems.
PNE is usually precipitated by prolonged sitting or trauma to the sitting area, combined with a genetic and developmental susceptibility. Each person’s body is unique. Tissue mass varies. Nerve routes vary. The amount of pressure a nerve can take before responding with inflammation varies. And so on. Putting all this together explains why some people can sit for 10 hours a day for 30 years and not get PNE, while someone else may sit 6 hours a day for 5 years and get it. However, some cases of PNE involve no prolonged sitting or trauma. Life has its mysteries….
PNE is common in high mileage bicyclists who do not stop cycling when the pain starts. It’s so common in this group it’s nicknamed Cyclist’s Syndrome. The prolonged sitting pressure, the continual nerve rubbing and stretching from pedal pumping, and the extremely high seat pressure on the ischial spine and perineum all combine to form the ideal conditions for PNE. Similarly susceptible groups are those using rowing machines or doing lots of sit-ups. The human body was simply not designed for these behaviors.
5. What is PN frequently misdiagnosed as?
PN is so rare and understanding of it is so recent that in most cases it goes misdiagnosed or undiagnosed for years. As one article says:
“Most patients felt hopelessly isolated as the world’s only victim of a malady without a name. Patients wondered whether their imagination was the source, but they knew it was not. They report that acquiring a name for their affliction and contacting other sufferers gave important help even while symptoms persisted.” – Source: –
PNE: Early Symptoms, Operative Techniques and Results.
It is important to understand that there could be other causes that have some similar symptoms and underlying conditions such as tumor and diseases of the spine or skin. It is most common that people with PN are diagnosed with chronic or non-bacterial prostatitis, prostadynia, vulvodynia, vestibulitis, interstitial cystitis, chronic pelvic pain syndrome, proctalgia, proctalgia fugax, orchialgia, hemorrhoids, coccydynia, piriformis syndromes, anorectal neuralgia, pelvic contracture syndrome/pelvic congestion, ischial bursitis, or levator ani syndrome. All of these above disorders can “mimic” Pudendal neuralgia symptoms or actually be caused by pudendal neuropathy.
Chris R, a PNE sufferer and former medical student at the Medical College of Georgia, US, and now a doctor, had this to say in 2002:
“Many PNE patients are originally diagnosed with one or multiple vague pelvic pain disorders before getting the correct diagnosis. The most common diagnoses are: prostatodynia, nonbacterial prostatitis, idiopathic vulvodynia (idiopathic means unknown cause), idiopathic orchialgia, idiopathic proctalgia, idiopathic penile pain, Levator ani syndrome, and coccydynia.
“The reason for these many diagnoses is that the pudendal nerves innervate urogenital and anorectal tissues, cutaneous (skin) tissue, and many small but very important muscles in the perineum. The muscles include: the external anal sphincter, puborectalis portion of the levator ani muscle, superficial and deep transverse perineus muscles, ischicavernosus, bulbospongiosus, and the external urethral sphincter.
“Irritation of the pudendal nerves can cause muscle spasms in one or more of the aforementioned muscles. Spasm of the external anal sphincter can cause constipation (anismus). Similarly, spasm of the external urethral sphincter can cause urinary hesitancy, mimicking prostatic problems. Spasm of any of the other muscles can cause discomfort and a feeling of tightness, cramping, etc.”
Some doctors have never even heard of pudendal neuralgia. So after numerous tests where the doctors can find nothing wrong, sometimes they assume that the problem must be psychosomatic and make referrals to counselors and psychiatrists. Unfortunately, sometimes people with pudendal neuralgia go through numerous doctors and tests before finally meeting up with a doctor who understands pudendal neuralgia and how to diagnose it. Sadly, often PN patients are told their problem is psychological.
6. How is PN correctly diagnosed?
Correct diagnosis follows these main stages:

A. The exam.
For guys the exam should include digital rectal exam. For ladies the exam should include a pelvic exam.
What is your history? Were you exercising heavily, did you have a pelvic surgery or vaginal delivery, were you sitting long hours? Is your pain in the distribution area innervated by the pudendal nerve? Is there increased pain or tenderness when your doctor presses along the course of the nerve via the rectum or vagina?

B. Elimination of other factors.
Often the pudendal nerve doctors recommend an MRI to rule out obvious problems such as tumors or spinal abnormalities. Each of the PN doctors has their own requirements on what type of MRI they prefer. It is also important to rule out other problems such as urinary tract infections, prostate infections, or sexually transmitted diseases. Disorders that might cause peripheral neuropathy such as Lyme’s disease or multiple sclerosis should also be ruled out. You should have a stool examination for possible blood. (Screen for colorectal cancer and other problems.) Guys should have a PSA.

C. Pelvic floor physical therapy that includes myofascial release.
If your doctor decides your problem might be PN often they will refer you to a physical therapist for pelvic floor physical therapy. It is difficult to distinguish between PNE and pelvic floor dysfunction (PFD) because typically PNE can cause PFD and the symptoms can be similar. A course of pelvic floor physical therapy can help to determine if you just have PFD. People with PNE are less likely to have good results from pelvic floor physical therapy.

D. Electrophysiological testing including EMG’s and PNMLT.
Results of these tests are not 100% accurate but they can help add to the overall picture as to how well the nerve is functioning. Sometimes, although not always, there will be a latency with the EMG and PNMLT testing that indicates a neuropathy. There are some doctors who rely mostly on the PNMLT and there are others who rely mostly on the EMG. Some doctors feel that utilizing the EMG, they can actually “tell” where the entrapment is.

E. Magnetic resonance imaging ( MRI), CT scan, and magnetic resonance neurography.
A 3 Tesla MRI using special settings and protocl may give clear enough images to see nerve entrapments in some cases. Magnetic resonance neurography (MRN) is similar to an MRI but it uses special software to enhance the image of small nerves that are difficult to see on a regular MRI. There are only a handful of centers in the world where you can have these tests and entrapments do not always show up so the test is only accurate for a diagnosis of PNE part of the time.

F. Pudendal nerve blocks.
If you experience significant pain relief for even a short time (several hours) from a nerve block that may mean you have pudendal neuralgia. However pudendal nerve blocks can temporarily ease the pain caused by other problems in the distribution area of the pudendal nerve so the nerve block is only one of the tools used in the diagnosis of PN.
None of the diagnostic tests for PN and PNE are 100% accurate so the more of these tests you have the better your overall picture will be in determining your diagnosis.
7. What should I do if I suspect I have PN or PNE?
- A. Find a doctor who knows something about it or is willing to learn — one who will make referrals for you and prescribe pain medications if needed. This might be your general practitioner. Often a pain management doctor will prescribe pain medications if you need them. Other specialties that are sometimes familiar with PN/PNE are gynecologists, urogynecologists, urologists, or neurologists. You may print out information from this website to take to your doctor.
- B. Avoid activities that aggravate your pain. You may have to make some lifestyle changes. At first this can be very difficult but it is important to avoid further damage to the nerve. Sitting, bending, or other hip flexion activities can cause further nerve damage and should be avoided. Since chronic pain can cause permanent changes in the spinal cord and brain it is important to try to keep your pain levels low. To aid in this see the medication section of this website under treatment options.
- C. Purchase a cushion for when you absolutely have to sit.
- D. Make sure your doctor rules out other possible illnesses such as an infections, cancer, or tumors. (See question 6.)
- F . If the pain does not improve or if it worsens, you may want to consider pudendal nerve blocks or try Botox injected into the pelvic floor muscles although there is debate in the medical community as to whether Botox should be tried prior to surgery.
-
G. If your pain continues and you have no quality of life you may want to consider surgery. You can choose to have an
intrathecal pain pump or
neurostimulator implanted. These may help to control your pain but may not offer a chance for the nerve to heal. The other surgical option is pudendal nerve decompression surgery but you will have to travel to see one of the PNE experts. They will most likely perform some tests and give you a series of nerve blocks. If they believe you have pudendal nerve entrapment you will have the option of
pudendal nerve decompression surgery.
If you have PN symptoms, you are in a tricky situation. There are so few experts in the world that you have only two basic choices: go see the experts or educate your doctor.
Do not postpone diagnosis and treatment. The longer the delay, the worse the pain tends to become. The longer and worse the pudendal nerve has been irritated, the less likely steroid injections are to be the cure, the more likely surgery will be needed, and the less likely surgery will be a complete success. This is because nerve damage, once it goes past a certain point, becomes irreversible. As one article says:
“Delay in diagnosis and treatment was the rule. Patients came to my attention an average of 7.3 years after onset (Range 0.5 to 20). Patients consulted urologists, gynecologists, neurologists, surgeons and internists on multiple occasions and reported little relief from treatments directed toward the anus, the bladder, the prostate and toward perineal muscle spasms. I record earliest symptoms because
delay is considered a source of treatment failure.” – Source:
PNE: Early Symptoms, Operative Techniques and Results.
8. Who are the PNE experts?
See the
list of physical therapists. Some physical therapists are specifically trained to evaluate and treat people with PN or PNE. Before traveling a long distance to a PNE physician there may be a trained physical therapist near you who can do a preliminary evaluation and treat you for pelvic floor dysfunction.
See the
list of doctors. Some of the PNE doctors give short free initial phone consultations. Some of them prefer to communicate by e-mail. Most of them require a series of 3 nerve blocks prior to PNE surgery and many of them like you to have at least one of the nerve blocks done by their team.
As PNE becomes more widely known in the medical profession, we can expect to see more experts emerge. The advantage of seeing an expert is you may avoid experiences like this one, from the archived Pudendal Neuropathy website’s Yahoo posts.
“Date: April 13, 2002. Please be careful, as colon & rectal specialists ARE SURGEONS. As another group member already stated, doctors are going to treat you in the area they are trained. After many other types of doctors, I went to one approximately 2 yrs. after my pain started, and he recommended a partial lateral sphincterotomy. This is literally cutting the sphincter muscle – in my case just one side because the great majority of my pain is on the left side. He told me he didn’t know about the vaginal pain but 95-98% “guaranteed” me I would no longer have rectal pain or burning. I can’t tell you how much worse this has made me and how much more difficult bowel movements have become! However, I am lucky not to have fecal incontinence! Ellen.”
9. How can I educate my doctor?
You may print off any material from this website or you can direct your physician to this website. This site can give your doctor a general overview of PN/PNE and can lead to avoidance of unnecessary treatment, avoidance of delay, and to the correct referrals.Those three things should be your goal.
Show them the following documents:

A. Fact sheet hand-out for medical professionals. Click
here.

B. This document.

E. Print the male or female pudendal nerve image in the
anatomy section and use it to discuss details of your pain with your doctor. Try to think and talk in terms of how nerve damage of some sort could be causing pain in specific nerve areas. Looking at the image, discuss how to diagnose your problem with specific tests at various places on the nerve. Also discuss how there are only four main ways to cure your pain if it’s PNE: pressure reduction (such as not sitting or sitting with special cushions), muscle reeducation, injections, and surgery. Use the image and documents to form a mental model of your case.

F. Then suggest they study the many documents, images, and material online at this site and others, unless they have a better source.

G.
At some point you may need to see an established expert. But these documents and this site can give your doctor a general overview of PN.
10. What should I do first? Stop making the problem worse.
The first thing to do is stop making the problem worse. Minimize your sitting time and when you do sit, sit on a cushion with a center cutout. This should be large enough to avoid pressure on the areas where pressure causes pain, and ideally the entire pudendal nerve area to be safe.
Don’t try to be a hero and “tough it out.” If you are a cyclist, stop that altogether. Minimize sitting like a fiend. This is called hyperavoidance of sitting. If you doubt the importance if this advice, just listen to the many tales of woe from those who sat a lot and now wish to high heaven they didn’t. The reason is excess sitting can cause irreversible nerve damage.
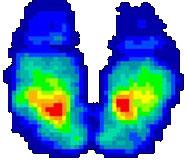
The two images below show typical pressure distribution patterns for sitting upright in chairs. Note the extreme pressure on the two ischial tuberosity bones, which normally carry about 75% of your weight when seated. This can be greatly reduced through use of contoured cushions or chair seats. Note there is less pressure in the central area. This can be further reduced with a trough or hole in the center of a sitting cushion. But the best thing to do is sit less.
You can tilt your seat angle forward about 8 degrees and/or lean forward. Both put more weight on the thighs and less on the problem area. Seat tilt is better because of the better back angle and reduced sheer pressure. Seat tilt can be accomplished with an adjustable chair, putting books or blocks under the back legs, or a wedge shaped piece of foam. A kneeling chair can be used for several hours a day for an even larger tilt, but this will probably require chair modification to use a better cushion. You can also consider the latest generation of office chairs or bicycles.
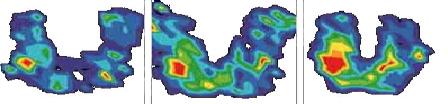
The three images on the left show the more even pressure distribution in the buttock area and the absence of high ischial pressure, with an appropriate cushion or chair.
There is no cushion or chair that works for everyone. Some PN’ers have used toilet seats and put canvas around it to sit. Others have bought high quality seat cushions which are more expensive while others have bought foam from their local store and made a U shape for their cushion. If you can keep pressure off of the pudendal nerve, any cushion would work fine. It might be worth looking into the different companies that offer U shaped cushions and select the one that you think may work for you. Some cushions have weight limits so be sure to read the manufacturers description of the cushion carefully and what the weight limits are. Large people may need a heavier and firm cushion while smaller individuals might be OK with a softer cushion. Just be sure to research before you buy.
Bicycle seats are now available for people with “cyclists syndrome”. The name of one of these seats is called a “horse saddle”. When looking for a good bicycle seat, you want to make sure that there is a cutout in the middle of the saddle of the seat, so it can take the pressure off of the nerve. All of the cushions and/or bicycle seats still need to be used in moderation, as some pressure may be put on the pudendal nerve while sitting.
11. What should I do second? Accept your condition.
The second thing to do is
accept your condition for what it is. Receipt of bad news causes a well known five step process in humans:
denial,
anger,
depression,
bargaining, and finally,
acceptance. This is the
Cycle of Acceptance. One usually bounces around between steps before finally getting to and remaining in full acceptance. If the bad news is minor the cycle will be swift and barely noticeable. If major, the cycle can take years or never be completed.
The reason you must come to accept your condition is that if you don’t, you will be less rational. This will cause two things: you will probably make your condition worse, and you will not be able to self manage your case very well. You will be stuck in the cycle and find yourself frustrated and angry at doctors who fail to help you, when what’s needed is a calm, cooperative, investigative attitude. If you find yourself angry or depressed much more than usual, you are stuck in the cycle. When it comes to mental clarity and happiness, it’s not the pain but the cycle that matters most.
While it’s true that the US medical system is full of doctors whose only goal is to get you out of the door in 15 minutes so they can see 2000 or so patients a year, it’s also true that no system is perfect, the one we have is much better than the one we had 100 years ago, and there are a few good doctors who care. The reason so many doctors are in a rush and assume they know all there is to know in their specialty is because the cost management side of the health care industry causes them to behave that way. The system is faulty, not the doctors.
The idea is to not blame others, which is scapegoating. Instead, don’t blame anyone. Rise above that low level of thinking and see the situation for what it is.
12. What should I do third? Develop a diagnostic plan.
The third thing to do is develop a diagnostic plan with your doctor. Remember now, you may or may not have PNE.
Here is a sample diagnostic plan but each case is different so this should be guided by your physician.

A. Have an MRI of the lower spine, pelvis, and sacrum. The PNE doctors each have their own protocol so while it is OK to have this done locally, before scheduling your MRI it is good to check with the PNE doctor you may eventually wish to see so that you know exactly what type of MRI they require. This can help you avoid having an MRI twice. Your local physicians may be willing to contact Dr. Hollis Potter for information on protocl and settings for the 3T MRI. You can find more information
here.

B. Rule out other conditions by having blood work to rule out other sources of peripheral neuralgia, like Lyme’s disease. (See question 6.)

C. Try all non invasive techniques first, like pelvic floor physical therapy and medications to help with neuropathic pain.

D. Have a pudendal nerve motor latency test (PNMLT) or other EMG tests.
If physical therapy is non effective, the medications are not giving you enough relief, and your quality of life is very low due to intense pain, then you may want to move on to option E.

E. If your pain is in the ischial area you could try a nerve block on the posterior cutaneous nerve. If the pudendal nerve seems to be the culprit you could try a pudendal nerve block.
The collection of all these tests is called a workup. An incomplete workup causes false assumptions, which can all too easily cause a false diagnosis, a guess, no diagnosis at all, or a wrong next stage plan. An excessive workup causes confusion, delay, and unnecessary expense. Only an expert can determine what a patient needs for a complete and non-excessive workup.
Some of the tests you need for a work-up can be done through your local physician but you may have to travel to a PNE expert for some of them.
Remember that most tests turn out normal and so serve only to rule out an area. Diagnosis proceeds just as a detective works: proof by elimination and revelation of cause and effect. Thus in a difficult case many, many tests are necessary.
Sherlock Holmes explained all this, the fine art of investigation, quite well in Sign of the Four, published in 1890. This is the source of one of his most famous quotes. (Now for some fun. Forget all your troubles for a moment. Italics have been added to highlight the quote. The all caps are in the original.)
“How came he, then?” I reiterated. “The door is locked, the window is inaccessible. Was it through the chimney?”
The grate is much too small,” he answered. “I had already considered that possibility.”
“How then?” I persisted.
“You will not apply my precept,” he said, shaking his head. “How often have I said to you that when you have eliminated the impossible whatever remains, HOWEVER IMPROBABLE, must be the truth? We know that he did not come through the door, the window, or the chimney. We also know that he could not have been concealed in the room, as there is no concealment possible. Whence, then, did he come?”
“He came through the hole in the roof,” I cried.
“Of course he did. He must have done so. If you will have the kindness to hold the lamp for me, we shall now extend our researches to the room above, the secret room in which the treasure was found.”
13. What is a nerve block?
In the context of PN, a nerve block involves injecting a liquid at a precise location near a nerve. For a small nerve like the pudendal that takes slightly different paths in different people, this requires more than just studying a person’s body and deciding where to insert the needle, at what angle, and how deep. While there are some physicians who give pudendal nerve blocks transvaginally or through the buttocks without using image guidance, most require imaging of some type, such as X-ray (fluoroscope), ultrasound, or CT. When image guidance is used, the needle enters in through the buttocks. Without the accuracy these imaging systems provide, it is difficult to know if the needle tip is located correctly. If incorrectly located, the nerve can be damaged or the injected liquid will be too far away to have its intended effect. Dr. Bensignor says the needle tip must be within one millimeter of the target. However, even with image guidance it is possible for the block to miss its mark.
There are two main types of injected liquids: a local anesthetic such as marcaine, and slow-release steroids. The local anesthetic is a short term diagnostic tool. If the pain is relieved for a few hours, the location was correct and the nerve can be suspected of being a contributor or even the sole source of pain. The steroids are a long term therapeutic attempt and in some cases they will decrease the nerve inflammation. This can take days or weeks, and improvement may be temporary or permanent. This delay explains why physicians prefer a delay of several weeks between nerve blocks with steroids. If the nerve is not irritated, the steroids have no effect. Some doctors use heparin, an anti-inflammatory medication, instead of steroids.
The most common sites for injection are at the ischial spine between the sacrotuberous and sacrospinous ligaments or in the Alcock’s canal. These are not the same as the blocks carried out for childbirth pain. Several physicians give nerve blocks into a 3rd location at the dorsal penile/clitoral branch of the pudendal nerve.
In some cases the blocks may worsen the pain for a few days or weeks. For a few people who have undergone nerve blocks, there has been a long-term worsening of symptoms including increased sitting pain or a condition called persistent genital arousal syndrome, possibly due to the nerve being “nicked” by the needle, a reaction to the medication, or formation of scar tissue.
It appears that steroids have less than a 5% chance of curing PNE. Of the many nerve blocks that Dr. Ken Renney’s team has done, they have “cured” only one patient with nerve blocks alone. This was a 17 year old male football player who had had the condition for only 3 weeks. After two injections he returned to football with “no discomfort.” As Ken wrote to one patient on 10/1/2003:
“We have only cured ONE person [with nerve blocks] since we started and I have seen about 150 patients. Not great stats but it’s the truth.”
This agrees with the generally low percentage rate seen in PN patients as a whole on the discussion forums. We were all scratching our heads. No one seemed to know anyone who had been cured by nerve blocks alone, though a few had seen a reduction in pain.
When the nerve block is conducted under guidance, the patient is asked to lie down in the prone position. Using a small needle the doctor injects an anesthetic to numb the buttocks prior to injecting with the larger needle that targets the pudendal nerve. When the doctor is able to find the pudendal nerve, he will then inject either the local anesthetic and the long term steroid or heparin. The procedure itself lasts approximately 30 minutes. This is done on an outpatient basis. No overnight stay is required.
If the injection relieves your pain that is considered a positive response to the nerve block and the pudendal nerve may be the source of your pain. If the injection did not provide any relief there are two possible conclusions.
1. The pain is not as a result of the pudendal nerve or
2. The physician did not get close enough to the pudendal nerve to feel any effects.
After a pudendal nerve block it is possible to evaluate whether the block hit the target of the pudendal nerve by testing the perineum, clitoral, and anal areas for loss of sensation and numbness. Sometimes the physician might order another block four to six weeks after your first block, to make sure that they can entirely rule out pudendal neuralgia, by trying to see if they can get close enough to the nerve again.
Occasionally medication from the nerve block can wander into the area of the sciatic nerve making it difficult for the patient to walk. This problem typically subsides within 24 hours.
Pudendal neuralgia: CT guided pudendal nerve block technique – This highly technical 1999 article describes the anatomy involved and how to perform nerve blocks. As the article says, “Infiltrations are made first at the ischial spine. If two consecutive nerve blocks into the ischial spine fail, a third injection can be made into the pudendal canal.”
Below are some great pictures of what to expect when receiving a nerve block. The first picture is a CT guided photo showing the optimum placement of the needle in this particular person.
Here is what one of the PNE experts says about nerve blocks:
“Most of the time in fact the compression of the nerve trunk is at the level of the claw between the sacro spinal and the sacro tuberal ligaments. That is why I don’t like to call this syndrome the Alcock syndrome, as far as mainly the compression is more important outside of the canal. Of course the Alcock tunnel syndrome does exist. That is why, according to the medical findings we start by blocks at the level of the claw. If it doesn’t work then we do the second block in the tunnel. The block at the level of the claw is done under fluoroscopy. The other one is scan guided under CT view. Two blocks can be done at each level on one or both sides but no more.”
“The second reason is that blocks constitute a very important diagnostic test. If they don’t work at all we can suspect a bad diagnosis. If they do well for a while (several days or weeks) they must be done another time. The surgical indications arise from the failure of those blocks with time. The main problem arises for patients without any effect after blocks. I do believe that then they are not candidates for surgery. A block which may lead to disparition of pain during some hours is nevertheless a good diagnostic test for us and may lead to surgery. So, the guideline could be as follow: Blocks at the two levels without any efficacy = bad diagnosis. Blocks at one or two levels with “long improvement” (some days or weeks ) = try one block again at the two levels. If it doesn’t work = surgery with very high hopes. Blocks with very short amelioration = surgery.”
14. What is the Pudendal Nerve Motor Latency Test (PNMLT)?
The full name is the pudendal nerve distal motor latency test. As the “Consensus Statement of Definitions for Anorectal Physiology and Rectal Cancer” for the United States defines it:
“Pudendal nerve latency is the measurement of the time from stimulation of the pudendal nerve at the ischial spine to the response of the external anal sphincter. Normal pudendal nerve terminal motor latency is <2.2 ms.”
This means the normal response time should be 2.2 milliseconds or less. Other points besides the ischial spine can be used for the test, which will cause a different response time. Dr. Robert’s approach uses several different points. The most common has a normal latency of 4.0 ms or less. As an example of PNMLT scores one patient’s results at Dr. Robert’s hospital were 4.7 ms left and 7.8 ms right.
Anything over the normal latency time means the nerve is not operating normally and is therefore probably damaged leading to motor dysfunction of the nerve. The pudendal nerve is found in the pelvis. Right and left branches of this nerve extend to the bladder and bowel sphincter muscles. When the nerves and muscles perform normally, we have control of bladder and bowel functions without discomfort. A problem with pudendal nerve function may lead to loss of control of the anal sphincter muscles. Such problems may cause leakage of urine or stool, conditions referred to as urinary incontinence and bowel incontinence. Problems with pudendal nerve and sphincter function may also cause chronic constipation or rectal pain.
The PNMLT does not measure the sensory function of the nerve but only measures the motor function of the nerve. So PNMLT scores do not necessarily correspond to pain levels. A recent publication reports that the PNMLT is not a good indicator of whether you have an entrapment but it may indicate a neuropathy.
Description of the PNMLT
The most widely used method of electrophysiological testing of pudendal nerve function is that described by Kiff and Swash at St. Mark’s Hospital in London. They used a rubber finger stall that has two stimulating electrodes at the tip and two surface electrodes for recording mounted three cm. proximally at its base. The index finger, mounted with the device, is inserted into the rectum and placed on the ischial spine. Electrical stimulation is then initiated and the latency of the response to the anal sphincter is recorded on surface or needle electrodes. The normal mean terminal latency is 2.0 +or – 0.3 msec. It must be pointed out that the pudendal nerve terminal motor latency test (PNTML) is solely a motor study, and is of importance only if the study is abnormal. In other words, the sensory nerve fiber component of the nerve more peripherally located can be compromised without involving the motor fibers. This anatomical situation can result in a patient with sensory fiber compression and pain having a negative PNTML test. In addition the test does not indicate the extent of injury or entrapment, but only if the nerve is responding abnormally. A comprehensive examination should include sensory nerve tests; as well as testing of the components of motor function, and EMG of the pelvic floor. With this information one could ascertain the severity of the damage i.e., if there is axonal damage or focal demyelization, determined by the motor amplitude and EMG characteristics; if the process is of recent or longstanding; and if there is an attempt to regenerate (needle EMG). Dr. Benson has developed a sensory testing method, based on the bulbo/clitorocavernosus reflex, in which a mild stimulus is applied to the glans penis or adjacent to the clitoris and the reflex conduction time to the pelvic floor muscle is measured. (
Weise, page 14)
PROCEDURE : You will be asked to undress from the waist down, and wear a patient gown with the opening in the back. A technologist trained in performing this exam will be conducting the test, and will explain everything he or she is going to do. You will be asked to lie on a stretcher, turn to your left side, and bend your knees. An electrode pad (similar to an EKG pad) will be placed on your buttock or thigh. The technician will then put on a rubber glove with an electrode on the index finger. After lubricating his index finger, he will gently insert it into your rectum. This should be no more uncomfortable for you than a rectal exam. The technologist will then send a mild, painless electrical stimulus through the electrode on his finger to your pudendal nerve. This stimulation may cause the muscles of your thigh to twitch involuntarily, but it will be painless. The technologist will then gently rotate his finger to repeat the test on the opposite branch of the nerve. A computer will record the response of your pudendal nerve to the stimulation. A physician will interpret the results and determine if any nerve conduction delays exist. The actual procedure will take 15-20 minutes.

This is a picture of the St. Marks electrode that is used to conduct the PNMLT.
15. What other electrophysiological tests are used to diagnose PN/PNE?
Some pudendal nerve physicians perform electrophysiological tests such as the sacral reflex test, cortical evoked potential test, and somatosensory evoked potential (SSEP) to test whether there is a problem in signals from the spinal cord and brain or in the motor responses of the pelvic floor . These tests usually require the use of electrodes or tiny needles inserted in muscles in the perineal area or in the forehead and small bursts of electrical stimulation. The tests can be slightly painful but do not last very long.
“An SSEP indicates whether the spinal cord or nerves are being pinched. It is helpful in determining how much the nerve is being damaged and if there is a bone spur, herniated disc, or other source of pressure on the spinal cord or nerve roots.” (see more information including
source at the page on
Spine Diagnostics SSEP)
Sacral reflex testing tests the motor response of muscles in the pelvic floor.
“Sacral reflexes consist of motor responses in the pelvic floor and sphincter muscles evoked by stimulation of sensory receptors in pelvic skin, anus, rectum, or pelvic viscera. These responses may be elicited by physical or electrical stimuli.”(
source)
One publication looks at the differences between the some of the more commonly used nerve testing.
Eric DeBisschop – Eric Bautrant
They look at “staged” sacral reflexes vs the Pudendal Nerve Motor Latency test. Many factors can interfere with nerve testing results. Examine with your doctor the pros and cons of using these tests.
16. Where is the pudendal nerve and what does it look like?
Some of the best anatomical images are the
Female Pudendal Nerve or
Male Pudendal Nerve. Study these images. Note the way the nerve branches out and covers a wide area. Is your pain located anywhere on the nerves shown? If so, and it gets worse with normal sitting and better sitting on a toilet seat,
and there is no apparent reason for the pain, you may have PNE.
Note how prominently the nerves stand out on the ischial spine. This is why prolonged sitting (especially heavy cycling) so frequently causes PNE. As Dr. Robert writes in his article, the pudendal nerve “describes a curve which drags it around the region of the ischial spine, which it straddles like a violin string on its bridge.”
Print the male or female image in normal or best mode, and in color. Circle the areas where your pain is. Now, what nerves are in those areas? Discuss this image with your doctor.
When you visit your doctor, ask to see and discuss additional images of the pudendal nerve.
What does the pudendal nerve look like? The image above is Figure 11 from
PNE by Dr. Robert. This photograph was taken after the surgical procedure that frees the pudendal nerve from entrapment by incisions on the sacrotuberal and sacrospinal ligaments, as discussed in the article.
An interesting image of the cutaneous nerve is at the
Gluteal Region. This is especially useful for those who do not have the classic PNE symptoms, but have sitting related pain in the ischial area and between the two ischial tuberosities.
17. Why does it take so long to feel better after surgery?
Patients are advised that it will be two to six weeks before they can return to work, depending out the physician and which type of surgery you had. This is just the surgery recovery period. For the pudendal nerve to return to its original normal pain-free condition usually takes much longer, generally several months to a year. However, some patients have felt huge reductions in pain as soon as they woke up after the operation.
Dr. Robert advises that a final assessment of the outcome of the surgery cannot be made until one year afterwards. He cautions that you should expect no improvement for the first three months and that most improvement occurs in the 3 to 12 months following surgery.
Some people have continued to see improvements in pain levels as long as 3 years after surgery. One reason for this is that nerves regenerate more slowly than many other tissues.
As Chris R explained:
“There are several reasons the nerve takes so long to get rid of the painful sensations:
“1. It takes a while to decrease the inflammation from the surgery.
“2. The damaged nerve has A LOT more receptors than a normal nerve making it A LOT more sensitive meaning it will conduct an impulse at a lower threshold. (hyperalgesia/allodynia) It takes a long time for these receptors to be down regulated. Taking 25mg of Elavil before going to bed every night is thought to block some receptors and speed up the process. I think it helps quite a bit. It can cause some constipation, though, so use some citrucel, etc if you use Elavil.
“3. The pain has been there a long time and the pathway is ‘grooved’ — it is called central nervous system plasticity. This is also thought to be helped some by low doses of Elavil. But most importantly, it takes A LOT of time.”
18. How can I learn more about PNE?
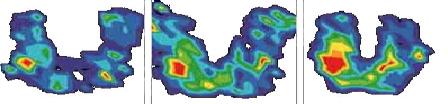 The three images on the left show the more even pressure distribution in the buttock area and the absence of high ischial pressure, with an appropriate cushion or chair.
The three images on the left show the more even pressure distribution in the buttock area and the absence of high ischial pressure, with an appropriate cushion or chair.


